Amerigroup TXPEC-1545-15 2016-2026 free printable template
Show details
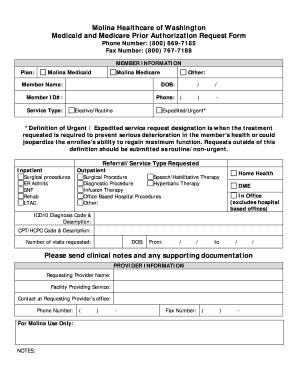
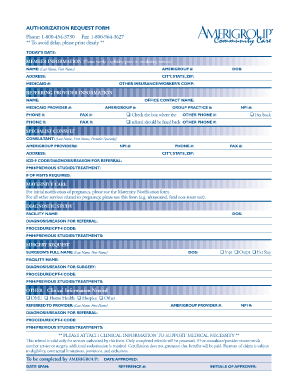
Precertification request Amerigroup prior authorization 1-800-454-3730 Fax 1-800-964-3627 To prevent delay in processing your request please fill out form in its entirety with all applicable information. Today s date Provider return fax Member information First name Last name Amerigroup member ID Address City State ZIP code DOB Contact Phone Additional member information Referring provider Participating Nonparticipating Full name NPI Provider ID Tax ID number TIN Office contact name Office...
pdfFiller is not affiliated with any government organization
Get, Create, Make and Sign precertification form

Edit your pre authorization form form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.

Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.

Share your form instantly
Email, fax, or share your pre certification form form via URL. You can also download, print, or export forms to your preferred cloud storage service.
How to edit printable medical prior authorization form template online
In order to make advantage of the professional PDF editor, follow these steps below:
1
Log into your account. In case you're new, it's time to start your free trial.
2
Upload a file. Select Add New on your Dashboard and upload a file from your device or import it from the cloud, online, or internal mail. Then click Edit.
3
Edit form precertification request form. Rearrange and rotate pages, add new and changed texts, add new objects, and use other useful tools. When you're done, click Done. You can use the Documents tab to merge, split, lock, or unlock your files.
4
Get your file. Select your file from the documents list and pick your export method. You may save it as a PDF, email it, or upload it to the cloud.
It's easier to work with documents with pdfFiller than you can have ever thought. You may try it out for yourself by signing up for an account.
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out a precertification request form is used to a copy through email phone or in person

How to fill out Amerigroup TXPEC-1545-15
01
Gather necessary patient information, including name, date of birth, and insurance details.
02
Fill out the patient's identifying information in the designated fields at the top of the form.
03
Specify the reason for the request in the appropriate section, including any relevant medical history.
04
Provide details about the services or items being requested, including codes if applicable.
05
Include the provider's information, including NPI number and contact information.
06
Make sure all required signatures are obtained, including the patient's and provider's.
07
Review the completed form for accuracy and ensure all fields are filled out correctly.
08
Submit the form via the designated submission method, whether electronically or by mail.
Who needs Amerigroup TXPEC-1545-15?
01
Individuals who are seeking healthcare services or items covered under Amerigroup insurance;
02
Healthcare providers who need to request authorization or referrals for their patients;
Fill
doc 0000015481 pdf
: Try Risk Free






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I modify precert without leaving Google Drive?
pdfFiller and Google Docs can be used together to make your documents easier to work with and to make fillable forms right in your Google Drive. The integration will let you make, change, and sign documents, like certification request form, without leaving Google Drive. Add pdfFiller's features to Google Drive, and you'll be able to do more with your paperwork on any internet-connected device.
How can I send documentation for precertification can include which of the following to be eSigned by others?
ameriben authorization form is ready when you're ready to send it out. With pdfFiller, you can send it out securely and get signatures in just a few clicks. PDFs can be sent to you by email, text message, fax, USPS mail, or notarized on your account. You can do this right from your account. Become a member right now and try it out for yourself!
Can I sign the ameriben precertification form electronically in Chrome?
Yes. You can use pdfFiller to sign documents and use all of the features of the PDF editor in one place if you add this solution to Chrome. In order to use the extension, you can draw or write an electronic signature. You can also upload a picture of your handwritten signature. There is no need to worry about how long it takes to sign your preauth form.
What is Amerigroup TXPEC-1545-15?
Amerigroup TXPEC-1545-15 is a specific form used for documenting and processing certain medical claims and authorizations in Texas under the Amerigroup health insurance program.
Who is required to file Amerigroup TXPEC-1545-15?
Healthcare providers and facilities that wish to submit claims for reimbursement or authorization requests to Amerigroup in Texas are required to file Amerigroup TXPEC-1545-15.
How to fill out Amerigroup TXPEC-1545-15?
To fill out Amerigroup TXPEC-1545-15, the provider must provide accurate patient information, details about the services rendered, relevant diagnosis codes, and any necessary documentation to support the claim or request.
What is the purpose of Amerigroup TXPEC-1545-15?
The purpose of Amerigroup TXPEC-1545-15 is to streamline the claims process, ensure proper documentation for services provided, and facilitate timely reimbursement for healthcare providers.
What information must be reported on Amerigroup TXPEC-1545-15?
The information that must be reported on Amerigroup TXPEC-1545-15 includes patient demographics, provider details, service dates, procedure codes, diagnosis codes, and any additional notes or attachments relevant to the claim.
Fill out your Amerigroup TXPEC-1545-15 online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Prairie States Prior Authorization Form Pdf is not the form you're looking for?Search for another form here.
Keywords relevant to american health holdings prior authorization form
Related to atip authorization form
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.